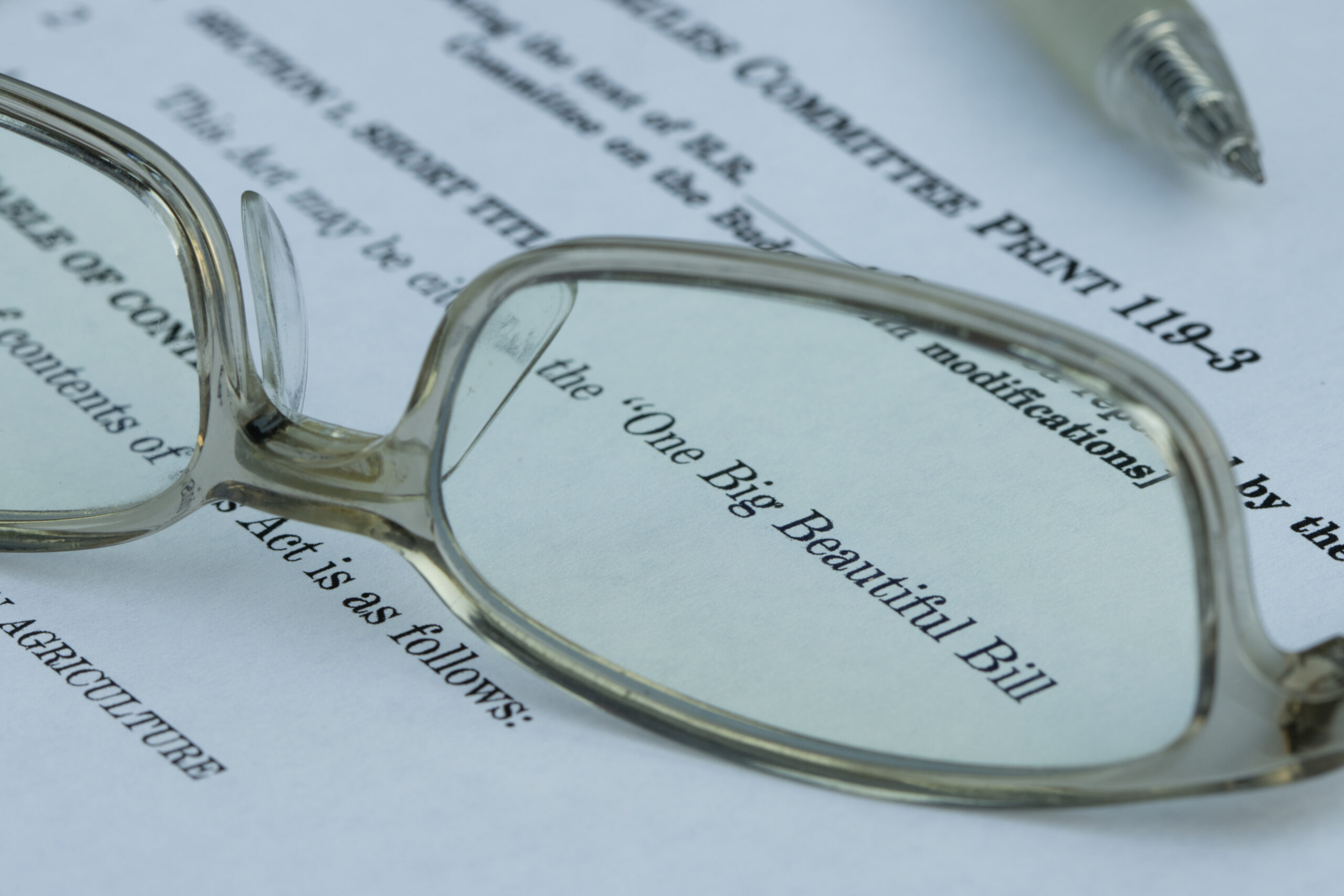
Key Factors that Drive Reimbursement in the PDPM Model
Dec 6, 2020
PDPM or Patient-Driven Payment Model is the new Medicare reimbursement system. It introduces a number of changes compared to the historical RUG-IV model. It is designed to address each patient’s unique needs independently and encourages more specialized, patient-driven care. Under PDPM, each patient is classified into a group of each of the five case-mix adjusted components. Those components include physical therapy, occupational therapy, speech-language pathology, non-therapy ancillary, and nursing.
PDPM classifies patients on their own characteristics to predict the therapy costs associated with that patient. For physical therapy and occupational therapy, two classifications are used—clinical and functional. Clinical is based on the primary diagnosis for the stay, while the functional score is derived from standardized assessment items such as bed mobility, eating, and walking, among others. In that same vein, speech-language pathology costs are also predicted by the model using patient characteristics. These characteristics include neurological clinical classification, SLP-related comorbidities, presence of cognitive impairment, use of a mechanically altered diet, or the presence of a swallowing disorder.
The non-therapy ancillary component is based on the presence of comorbidities or the use of certain extensive services. These comorbidities and extensive services are derived from a variety of MDS sources, including the ICD-10-CM codes.
The final component of the new model is nursing. Aside from a few modifications, PDPM utilizes the same basic nursing classification structure as the historical RUG-IV model.
The first modification involves creating a function score based on Section GG of the MDS 3.0, while another modification includes the collapsing of functional groups to a reduced number of 25.
Another key factor in the PDPM model is the variable per diem adjustment. This adjustment accounts for changes in resource utilization throughout the stay. Under this new model, the adjusted per diem rate is designed to decline the longer patients stay
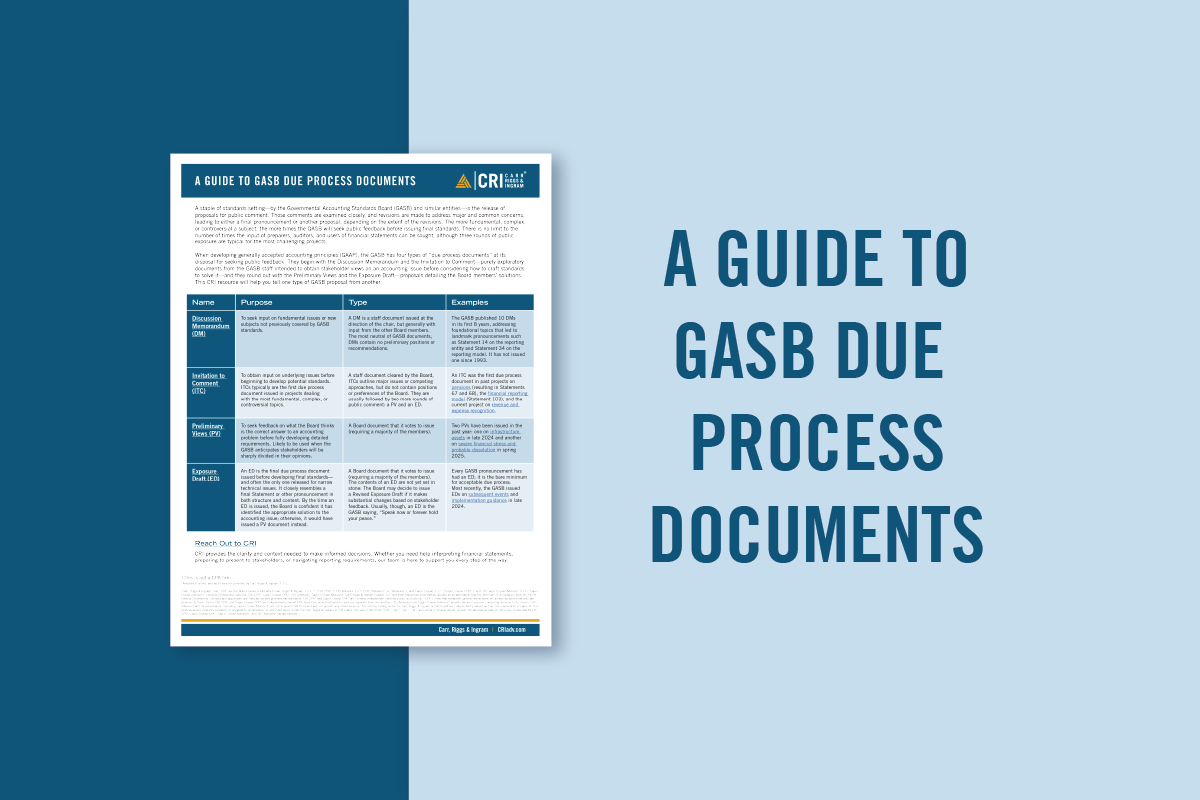
Since reimbursement is the driver of the long-term care industry, these new changes can be a bit confusing to understand and implement. If you’re looking to assess the implementation of this new model, contact a CRI advisor to see how you can make it more profitable in your setting.